Santati IVF
Little Heart Hospital Offers Advanced IVF Care
IVF at Little Heart Hospital is dedicated to providing comprehensive fertility care with advanced technology and compassionate support. Our highly skilled fertility specialists offer personalized treatment plans tailored to the unique needs of each patient, ensuring the best possible outcomes. The unit is equipped with cutting-edge facilities and technologies, making it a trusted destination for families seeking fertility solutions.
IUI (Intrauterine Insemination)
IUI is a fertility treatment where sperm is directly inserted into a woman’s uterus to increase the chances of fertilization. This procedure is timed with ovulation, helping the sperm get closer to the egg. It is often recommended for couples with unexplained infertility, mild male infertility, or issues with cervical mucus. IUI is minimally invasive and a cost-effective option for couples trying to conceive. The process involves monitoring ovulation, preparing the sperm sample, and performing the insemination in a controlled environment to enhance the likelihood of pregnancy.


Fertility Check-up
A fertility check-up is a comprehensive assessment of both male and female reproductive health. For women, it includes hormone tests, ultrasound scans, and ovarian reserve evaluation to check egg health. For men, it involves semen analysis to assess sperm count, motility, and morphology. This check-up helps identify underlying causes of infertility, such as hormonal imbalances, structural abnormalities, or issues with ovulation. By diagnosing problems early, a fertility check-up provides a clear pathway for creating a personalized treatment plan, improving the chances of a successful pregnancy.
Ultrasound
Ultrasound is a key diagnostic tool in fertility treatments, providing detailed images of the uterus, ovaries, and other pelvic organs. It is used to monitor follicle growth during ovulation, assess endometrial thickness, and detect abnormalities like cysts or fibroids. In fertility treatments like IVF and IUI, ultrasound guides procedures such as egg retrieval and embryo transfer. It also plays a critical role in early pregnancy monitoring to ensure proper development. Ultrasound is a non-invasive and safe way to track reproductive health and optimize fertility outcomes.

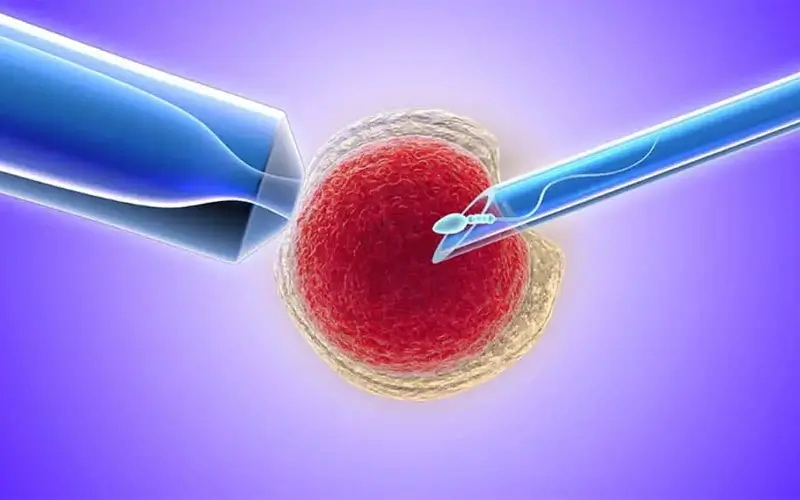
IVF/ICSI (In Vitro Fertilization/Intracytoplasmic Sperm Injection)
IVF involves retrieving eggs from the ovaries and fertilizing them with sperm in a laboratory. Once the embryo develops, it is transferred into the woman’s uterus. ICSI, a specialized form of IVF, is used when male infertility is a factor, where a single sperm is injected directly into the egg to enhance fertilization. Both IVF and ICSI are effective treatments for a variety of infertility issues, including blocked fallopian tubes, ovulation disorders, and severe male infertility, offering couples a high chance of conception and successful pregnancy.
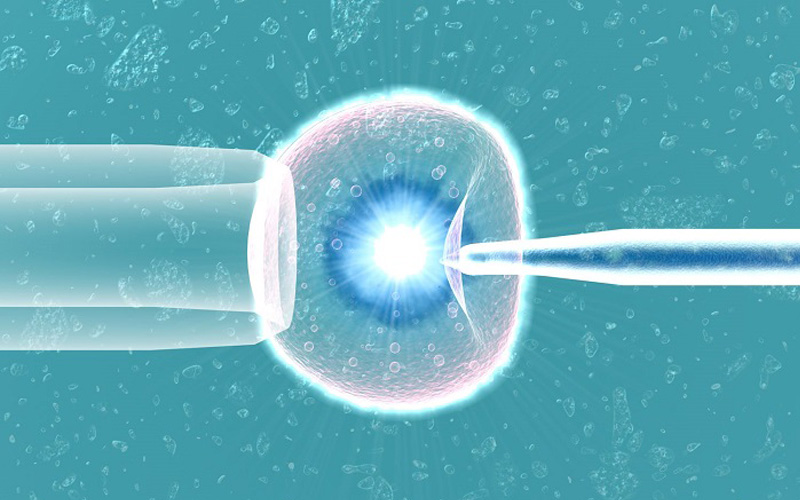
Laser Assisted Hatching
Laser-assisted hatching is a technique used in IVF to enhance embryo implantation. The process involves using a laser to create a small opening in the embryo’s outer shell (zona pellucida), which helps the embryo hatch and attach to the uterine lining. This method is particularly beneficial for patients with previous failed IVF cycles, women of advanced maternal age, or those with poor embryo quality. By improving the chances of implantation, laser-assisted hatching can increase the likelihood of a successful pregnancy in assisted reproductive treatments.

Blastocyst Culture
Blastocyst culture is the process of growing embryos in a lab for five to six days until they reach the blastocyst stage, a more developed phase compared to the traditional three-day embryo transfer. By allowing embryos to develop to this stage, doctors can better select the most viable ones for transfer, increasing the chances of implantation and successful pregnancy. This technique is often used in IVF cycles to improve pregnancy rates, especially for patients with multiple failed IVF attempts or those undergoing pre-implantation genetic testing.
Laparoscopy
Laparoscopy is a minimally invasive surgical procedure used to diagnose and treat conditions affecting fertility, such as endometriosis, fibroids, or blocked fallopian tubes. A small camera (laparoscope) is inserted through a tiny incision in the abdomen, allowing the doctor to view the reproductive organs and perform necessary procedures without large incisions. Laparoscopy is often used to correct abnormalities that can impact fertility, improving the chances of conception either naturally or with assisted reproductive technologies like IVF. It is a safe and effective option with minimal recovery time.

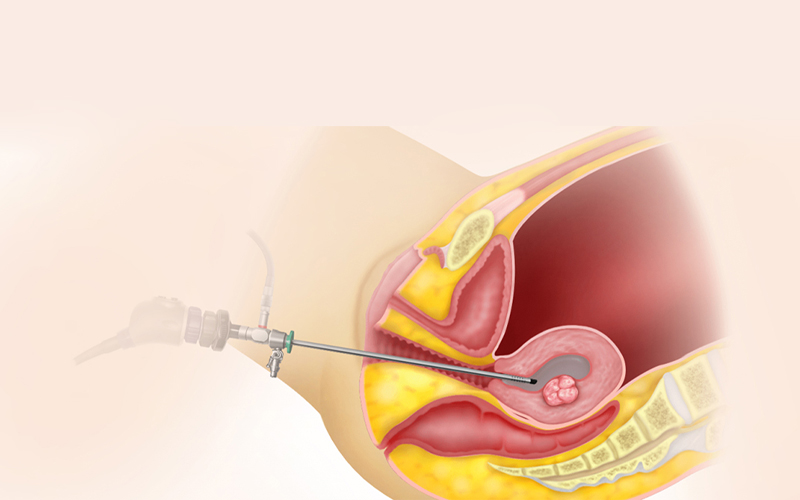
Hysteroscopy
Hysteroscopy is a minimally invasive procedure used to examine and treat the inside of the uterus. A thin, lighted tube (hysteroscope) is inserted through the cervix to identify abnormalities such as fibroids, polyps, adhesions, or structural issues that may affect fertility or cause miscarriage. In addition to diagnosis, hysteroscopy can be used to perform corrective surgery, improving the chances of successful pregnancy. It is a highly effective procedure with a short recovery time, and it plays an important role in fertility treatments, especially for women experiencing repeated implantation failure.
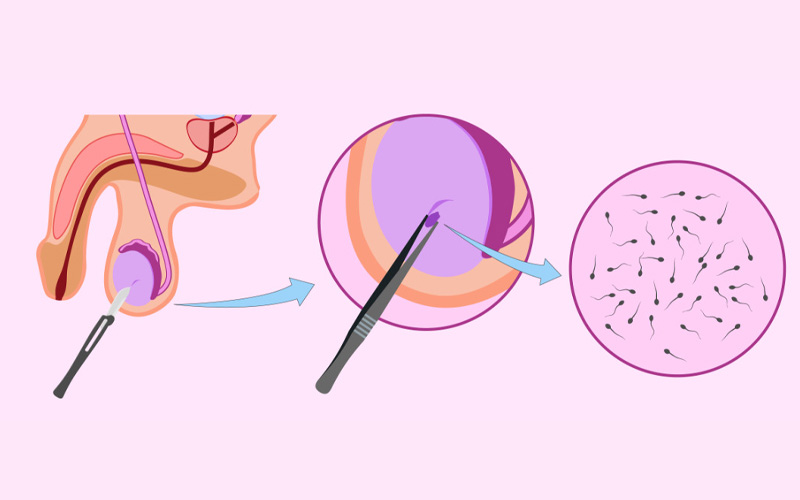
TESA/TESE (Testicular Sperm Aspiration/Extraction)
TESA (Testicular Sperm Aspiration) and TESE (Testicular Sperm Extraction) are surgical procedures used to retrieve sperm directly from the testicles in men with severe male infertility. These procedures are typically used when sperm cannot be found in the ejaculate due to blockages or other issues. The retrieved sperm can then be used in assisted reproductive techniques like ICSI to fertilize an egg. Both procedures are minimally invasive and provide an opportunity for men with infertility issues to father biological children.

Male Infertility Treatment
Male infertility treatment focuses on diagnosing and treating conditions that affect sperm production, quality, or delivery. Treatments may include medications to address hormonal imbalances, lifestyle changes to improve sperm health, or surgical interventions to correct blockages or other physical issues. Advanced procedures such as TESA/TESE can be used to retrieve sperm directly from the testes. Male infertility is a contributing factor in many infertility cases, and with proper diagnosis and treatment, many men can successfully father children through assisted reproductive technologies.
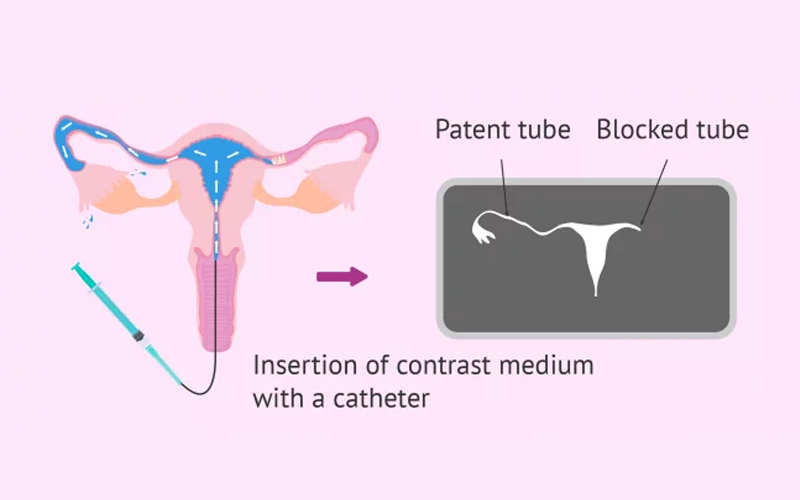
HSG (Hysterosalpingography)
Hysterosalpingography (HSG) is a diagnostic X-ray procedure used to evaluate the shape of the uterus and the openness of the fallopian tubes. During the procedure, a contrast dye is injected into the uterus, and X-rays are taken to track the dye’s flow through the reproductive organs. HSG is commonly used to detect blockages in the fallopian tubes or abnormalities in the uterus that may be causing infertility or recurrent miscarriages. It is an important tool in fertility evaluations, helping doctors determine the best course of treatment for patients.